JENNIFER RIGBY, NATALIE GROVER and MAGGIE FICK, of Reuters, report on how efforts to roll-out the world’s first malaria vaccine are being thwarted…
London, UK/Kisumu, Kenya
Reuters
After decades of work, the World Health Organization endorsed the first-ever malaria vaccine last year – a historic milestone that promised to drive back a disease that kills a child every minute.
In reality, efforts are falling well short of that, with a lack of funding and commercial potential thwarting GSK Plc’s capacity to produce as many doses of its shot as needed, according to Reuters interviews with about a dozen WHO officials, GSK staff, scientists and non-profit groups.

A nurse administers the malaria vaccine to an infant at the Lumumba Sub-County hospital in Kisumu, Kenya, on 1st July. PICTURE: Reuters/Baz Ratner
The British drugmaker committed to produce up to 15 million doses every year through 2028, following 2019 pilot programs – considerably less than the WHO says is needed. It is currently unlikely to make more than a few million annually before 2026, according to a source close to the vaccine rollout.
A GSK spokesperson told Reuters that it could not make enough of its vaccine Mosquirix to meet the vast demand without more funds from international donors, without giving details on the numbers of doses it expected to produce annually in the first years of the roll-out.
“Mosquirix has the potential to save a lot of precious lives before another new vaccine arrives. The more we wait, the more children die needlessly.”
– Kwame Amponsa-Achiano, a public health specialist leading a pilot vaccination program in Ghana.
“Demand over the next five to 10 years will probably outstrip the current forecasts on supply,” said Thomas Breuer, GSK’s chief global health officer.
The vaccine’s effectiveness at preventing severe cases of malaria in children is relatively low, at around 30 per cent in a large-scale clinical trial. Some officials and donors are hoping that a second shot being tested by Oxford University may prove better, cheaper and easier to produce in bulk.
Yet the world’s inability to fund more Mosquirix shots dismays many in Africa. Children on the continent account for the vast majority of the roughly 600,000 global malaria deaths every year.
“Mosquirix has the potential to save a lot of precious lives before another new vaccine arrives,” said Kwame Amponsa-Achiano, a public health specialist leading a pilot vaccination program in Ghana. “The more we wait, the more children die needlessly.”
Rebecca Adhiambo Kwanya in the Kenyan city of Kisumu needs no convincing: her four-year-old child Betrun has suffered numerous malaria bouts since birth, yet her 18-month-old Bradley – vaccinated in the pilot program – hasn’t caught it.
“My elder one was not vaccinated and he was sick on and off,” she said. “But the smaller one, he got the vaccine and he was not even sick.”

Rebecca Adhiamba Kwanya, 29, poses for a photo with her sons Betrun, four, and 18-month-old Bradley, at their home in Kisumu, Kenya, on 1st July. PICTURE: Reuters/Baz Ratner
The limited international appetite to produce and distribute more Mosquirix stands in stark contrast to the record speed and funds with which wealthy countries secured vaccines for COVID-19, a disease that poses relatively little risk to children.
Unlike many pharmaceutical products, there is no major market for a malaria vaccine in the developed world, where drug companies typically make the large profits that they say allows them to make their products available at far lower prices in poorer countries.
“This is a disease of the poor, so it’s not been that appealing in terms of the market,” said Corine Karema, chief executive of the non-profit RBM Partnership to End Malaria, which is working with governments in Africa to eliminate the disease.
“But one kid dies of malaria every minute – that’s unacceptable.”
In the coming weeks, global health organisations will announce the next steps to make Mosquirix widely available, including the first procurement deal and the WHO’s recommended allocation to prioritise roughly 10 million children at highest risk, the source familiar with the rollout plans said.
Long-term, WHO officials say roughly 100 million doses a year of the four-dose vaccine will be needed, which would cover around 25 million children. When the UN agency backed Mosquirix last October, it said that even a smaller supply could save 40,000 to 80,000 lives each year, without specifying the number of doses required.
GSK’s maximum target of 15 million doses could prevent up to about 20,000 deaths each year, according to a Reuters review of the malaria vaccine models used by WHO.
Yet even hitting 15 million could take years, according to several officials at the WHO and elsewhere in the malaria effort who said wider distribution beyond the pilot countries was unlikely before early 2024, and even then it would start slowly.
GSK also has to upgrade its manufacturing capacity to reach its target. It said it had set up a funding deal with international vaccine alliance Gavi to help stockpile a key ingredient of the shot to ensure there was no gap in supply during that process.
“We are on course to complete the agreed stockpiling volume,” said a spokesperson.
The drugmaker £700 million in the vaccine’s development and says it won’t charge more than five per cent above the cost to produce it.
“No company wants to be in a situation where you build manufacturing which oversupplies the market and vaccines will not be used,” said Breuer said, referring to a future split in demand between Mosquirix and the Oxford vaccine, if approved.
After 2028, India’s Bharat Biotech will take over production of Mosquirix’s key ingredient.
GSK’s Breuer expects the deal with Bharat to accelerate production. The British drugmaker will continue to produce the adjuvant – immune-boosting portion – of the vaccine, and recently committed to doubling production to 30 million doses annually, without offering a timeline.
Bharat Biotech, which has yet to outline its manufacturing plans, did not respond to requests for comment.
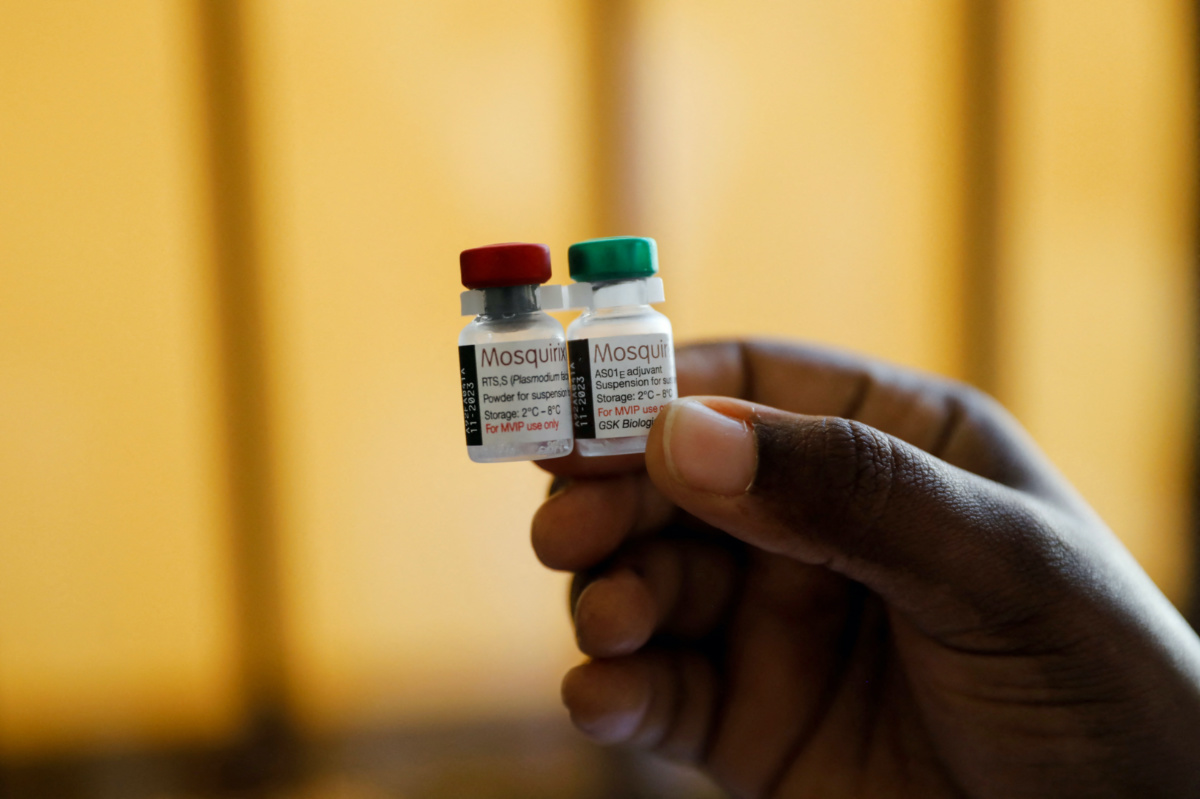
A nurse holds malaria vaccine vials before administering it to an infant at the Lumumba Sub-County hospital in Kisumu, Kenya, on 1st July. PICTURE: Reuters/Baz Ratner
GSK has donated 10 million doses to pilot programs in Ghana, Kenya and Malawi, and less than half have been shipped so far. The countries plan to expand campaigns this year and next using a mix of the remaining donations and purchased shots.
GSK said a WHO decision to collect additional data on safety and effectiveness from the pilot programs had added years to the launch process, during which it had to idle a dedicated production facility.
The WHO said safety questions had to be addressed before approval, and that it was working urgently to boost supply.
Mary Hamel, the agency’s malaria vaccine implementation head, told Reuters that COVID vaccines had shown how quickly things could move with the political will and funding – which she said malaria had never had.
Mosquirix has been in development since the 1980s, in part because of the complexity of targeting the malaria parasite.
Its regulatory pathway has also been slow. In 2015, GSK published results from a large-scale clinical trial showing vaccine reduced the risk of severe malaria by about 30 per cent. The WHO sought more data on the shot’s safety and effectiveness, gathering information from 2019 during the pilot vaccination programs, before endorsing Mosquirix.
In the past, such real-world data on a vaccine has often been tracked after it has been authorized for use.
“Would we have done it in the West? I don’t know,” said WHO’s Hamel, who was not involved in the decision, referring to holding up the deployment of shots to collect extra data.
We rely on our readers to fund Sight's work - become a financial supporter today!
For more information, head to our Subscriber's page.
Now recommended for use, it is not clear how the shot’s distribution will be financed long-term. Funding for malaria totaled $US3.3 billion in 2020, less than half of the estimated need, the WHO said, for tools such as treatments, bed nets and insecticides.
Adding malaria vaccines could cost between $US325 million and more than $600 million annually, depending on how widely they are used, according to a study by global health researchers published in the Lancet journal in 2019. The WHO estimates that the GSK vaccine will cost around $US5 per dose.
Two of the biggest funders behind the development and pilot programs for Mosquirix, the Bill and Melinda Gates Foundation and the Global Fund to Fight AIDS, Tuberculosis and Malaria, told Reuters they were committing almost no additional financing to deploy the vaccine.
“It’s not a silver bullet, and it’s relatively expensive compared to other interventions used for malaria,” said Peter Sands, head of the Global Fund. “The fundamental issue with malaria isn’t actually about tools. It’s about the fact that we spend far too little money on it.”
The Gates Foundation said it would continue to back research into how to best use the “historic” vaccine, but “concerns about the relatively low efficacy, short duration, and constrained supply challenges” meant it would not fund deployment.
Gavi is currently the only significant source of funding for a wider Mosquirix rollout. It has approved about $US155 million for 2022 through 2025, alongside some funding from the countries themselves. Internal documents seen by Reuters suggest Gavi’s investment in the first year is only expected to be $US20 million.
A source familiar with the plans said the group hoped that getting the vaccine rolled out, and countries showing demand, would make the case for more investment.
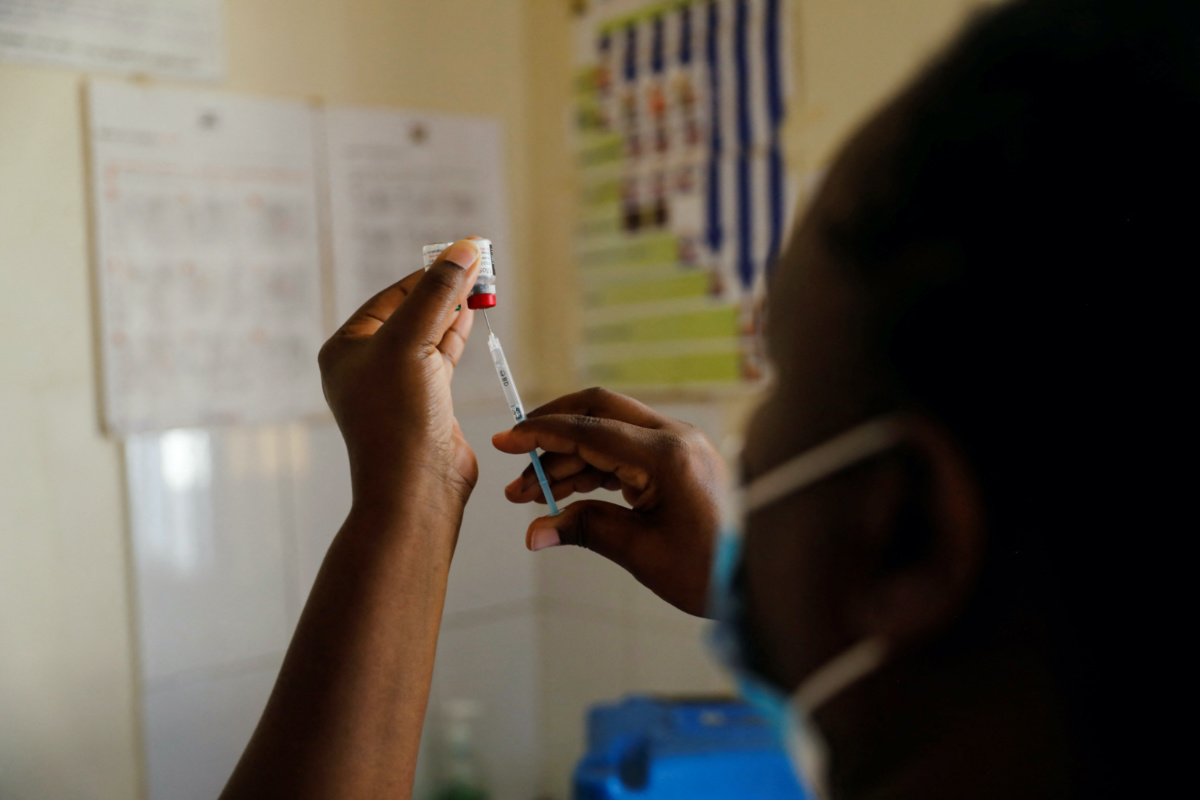
A nurse fills a syringe with malaria vaccine before administering it to an infant at the Lumumba Sub-County hospital in Kisumu, Kenya, on 1st July. PICTURE: Reuters/Baz Ratner
Several global health officials said future funding from donors might be better committed to a new shot from the scientists at Oxford University who developed AstraZeneca’s COVID vaccine.
Data from small trials showed 77 per cent efficacy over a 12-month period, if given to babies shortly before the peak malaria season. Results from a much larger clinical trial are expected in the coming weeks. Some researchers suggest the GSK vaccine, too, may show higher effectiveness if given seasonally.
Oxford scientist Adrian Hill told Reuters his team aims to secure a WHO recommendation for their malaria shot within a year of submitting data to the agency.
The Serum Institute of India, which will manufacture the vaccine, told Reuters it expects to be able to make up to 200 million doses annually by the end of 2024.
In the years ahead, there are also hopes for a shot being developed by BioNTech, using the same mRNA technology as their successful COVID vaccine made with Pfizer. BioNTech aims to begin human trials by the end of 2022.
But in the years before either of those shots might be used, there will not be enough vaccines even for those 10 million children the WHO says are most at risk.
“We should have had this vaccine a long time ago,” said Alassane Dicko, professor of public health at the University of Science, Techniques and Technologies of Bamako in Mali, who has led some of the Mosquirix trials.
“We have to do more.”