London, UK
Reuters
Gilead’s remdesivir should not be used for patients hospitalised with COVID-19, regardless of how ill they are, as there is no evidence the drug improves survival or reduces the need for ventilation, a World Health Organization panel said on Friday.
“The…panel found a lack of evidence that remdesivir improved outcomes that matter to patients,” the guideline said.
“Especially given the costs and resource implications associated with remdesivir…the panel felt the responsibility should be on demonstrating evidence of efficacy, which is not established by the currently available data,” it added.
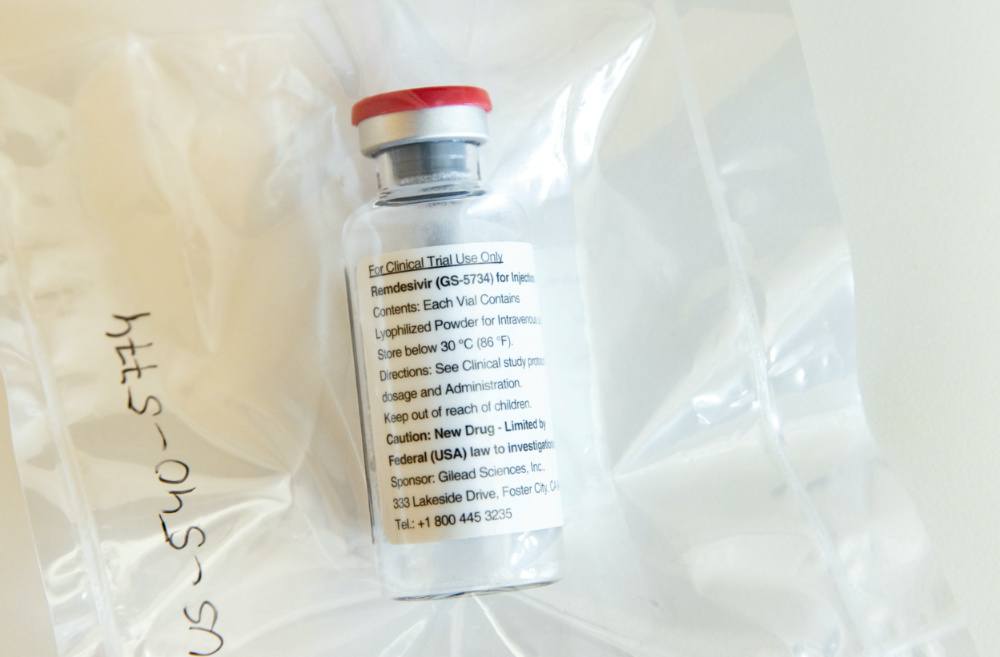
An ampule of Gilead Sciences’ COVID-19 antiviral remdesivir is pictured during a news conference at the University Hospital Eppendorf (UKE) in Hamburg, Germany, on 8th April. UPICTURE: Ulrich Perrey/Pool via Reuters
The advice is another setback for the drug, which grabbed worldwide attention as a potentially effective treatment for COVID-19 in the summer after early trials showed some promise.
The antiviral, known by the brand name Veklury, is one of only two medicines currently authorised to treat COVID-19 patients across the world. But a large WHO-led trial known as the Solidarity Trial showed last month that it had little or no effect on 28-day mortality or length of hospital stays for COVID-19 patients.
COVID-19 REINFECTION UNLIKELY FOR AT LEAST SIX MONTHS, STUDY FINDS
People who’ve had COVID-19 are highly unlikely to contract it again for at least six months after their first infection, according to a British study of healthcare workers on the frontline of fight against the coronavirus pandemic.
The findings should offer some reassurance for the more than 51 million people worldwide who have been infected with the pandemic disease, researchers at the University of Oxford said.
“This is really good news, because we can be confident that, at least in the short term, most people who get COVID-19 won’t get it again,” said David Eyre, a professor at Oxford’s Nuffield Department of Population Health, who co-led the study.
Isolated cases of re-infection with COVID-19, the disease caused by the SARS-CoV-2 virus, had raised concerns that immunity might be short-lived and that recovered patients may swiftly fall sick again.
But the results of this study, carried out in a cohort of UK healthcare workers – who are among those at highest risk of contracting COVID-19 – suggest cases of reinfection are likely to remain extremely rare.
“Being infected with COVID-19 does offer protection against re-infection for most people for at least six months,” Eyre said. “We found no new symptomatic infections in any of the participants who had tested positive for antibodies.”
The study, part of a major staff testing programme, covered a 30-week period between April and November, 2020. Its results have not peer-reviewed by other scientists but were published before review on the MedRxiv website.
During the study, 89 of 11,052 staff without antibodies developed a new infection with symptoms, while none of the 1,246 staff with antibodies developed a symptomatic infection.
Staff with antibodies were also less likely to test positive for COVID-19 without symptoms, the researchers said, with 76 without antibodies testing positive, compared to only three with antibodies. Those three were all well and did not develop COVID-19 symptoms, they added.
“We will continue to follow this cohort of staff carefully to see how long protection lasts and whether previous infection affects the severity of infection if people do get infected again,” Eyre said.
– KATE KELLAND, Reuters
The medication was one of the drugs used to treat US President Donald Trump’s coronavirus infection, and had been shown in previous studies to have cut time to recovery. It is authorised or approved for use as a COVID-19 treatment in more than 50 countries.
Gilead has questioned the Solidarity Trial’s results and said in a statement on Friday it was “disappointed” at the new WHO guideline.
“Veklury is recognised as a standard of care for the treatment of hospitalised patients with COVID-19 in guidelines from numerous credible national organisations,” it said.
The WHO advice raises questions about whether the European Union will need the 500,000 courses of the antiviral, worth a billion euros, it ordered last month.
The European Commission said on Friday it had taken note of the WHO updated guideline on remdesivir but that “at the moment, there are no changes” to its authorisation for the drug.
It said the region’s drugs regulator, the European Medicines Agency, had requested the full data from the Solidarity Trial and “will assess the evidence…together with other available data, to see if any changes are needed”.
Italy’s drugs regulator, AIFA, said it had been “stressing for weeks the modest effectiveness of remdesivir”.
“In practice we have been saying for some time that it is not of use for much,” a spokeswoman said.
No meaningful effect
The WHO’s Guideline Development Group panel said its recommendation was based on an evidence review that included data from four international randomised trials involving more than 7,000 patients hospitalised with COVID-19.
After reviewing the evidence, the panel said it concluded that remdesivir, which has to be given intravenously and is therefore costly and complex to administer, has no meaningful effect on death rates or other important outcomes for patients.
Peter Horby, a professor of emerging infectious diseases at Britain’s Oxford University, said the WHO’s new advice should prompt “a rethink about the place of remdesivir in COVID-19”.
“Remdesivir is an expensive drug that must be given intravenously for five to 10 days, so this recommendation will save money and other healthcare resources,” he said.
US infectious disease doctors said they would continue to use the drug because a double-blind, placebo-controlled US study showed it decreased the length of hospitalisation for some COVID-19 patients.
“My perspective is, and our institution’s perspective, is that this is still a useful drug. It’s not as useful as we’d like it to be,” Dr Rajesh Gandhi, an infectious diseases physician at Massachusetts General Hospital and Harvard Medical School, said.
Dr Helen Boucher, chief of geographic medicine and infectious diseases at Tufts Medical Center in Boston, said she was taking into consideration that the Solidarity trial was an open label study – meaning doctors and patients were aware that the drug was given – and not a double-blind, placebo-controlled study. Placebo-controlled studies are generally considered more scientifically rigorous.
The recommendation, which is not binding, is part of the WHO’s so-called “living guidelines” project, designed to offer ongoing guidance for doctors. The panel added that it supported continued enrolment into clinical trials evaluating remdesivir in patients with COVID-19, which it said should “provide higher certainty of evidence for specific groups of patients”.